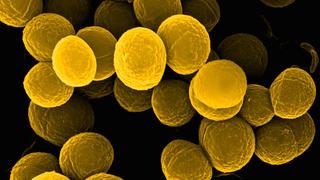
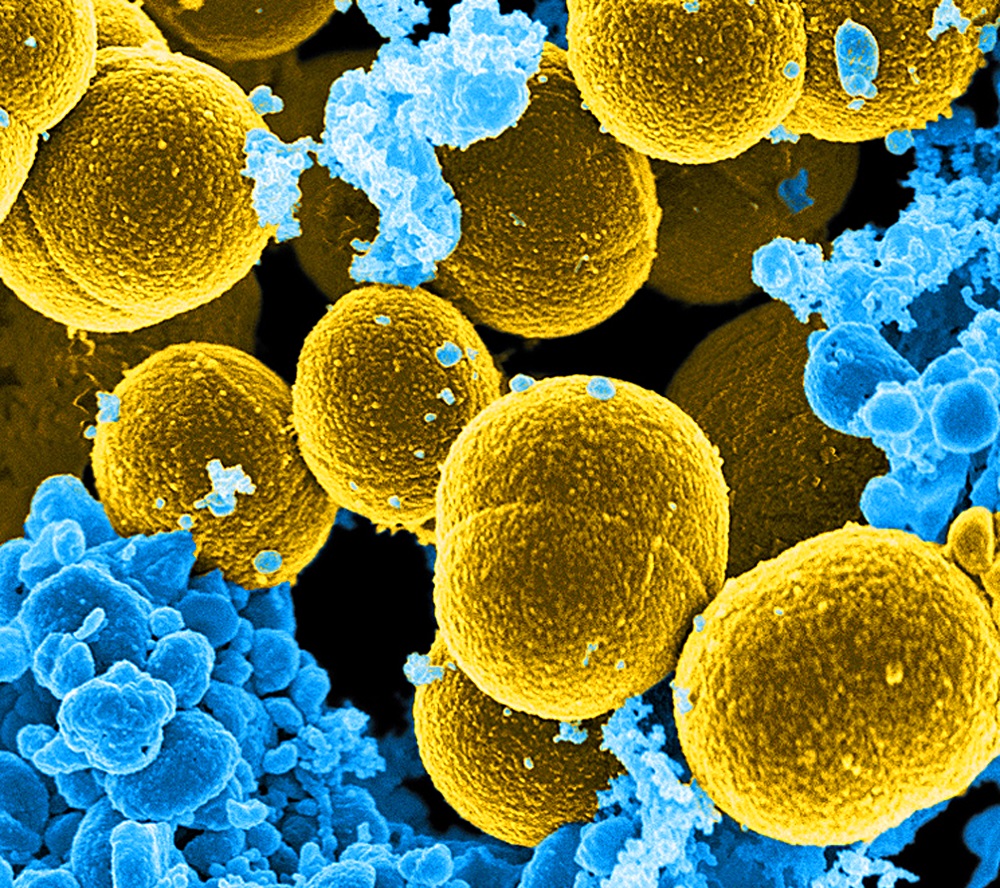
Staphylococcus aureus is a type of gram-positive bacteria that is responsible for more than half of all Staphylococcal infections.
Heavy growth of Staphylococcus aureus can cause skin infections like impetigo, scalded skin syndrome, osteomyelitis, septic arthritis, endocarditis, thrombophlebitis, toxic shock syndrome, sepsis, and a host of
other infections.
The laboratory establishes the heavy growth of Staphylococcus aureus in a sample when the bacteria occupy all the areas of the culture plate.
This happens after Staphylococcus aureus has replicated through binary fission, therefore leading to an increase in the number of bacteria and subsequently the heavy growth of the organism.
What Does Heavy Growth of Staphylococcus aureus mean?
- Heavy growth of Staphylococcus aureus is established in the Laboratory when the bacteria occupy all areas of the culture plate.
- Laboratory reports of bacteria will report Staphylococcus aureus bacteria as present in either ‘heavy’ growth, ‘moderate’ growth, or ‘scanty’ growth. Some cases establish isolate as a pathogen.
- The amount of growth of Staphylococcus aureus bacteria in a sample is not always directly proportional to the degree of infection in a patient. Test results establishing scanty growth do not typically mean a low degree of infection, as other factors can determine the amount of growth on the culture plate.
- Contamination of the sample, poor culture-collection technique, prior use of antibiotics by the patient, and wound dressings are some of the factors that can affect the amount of growth of Staphylococcus aureus bacteria in a sample.
- External factors affecting the test sample report do not mean testing is insignificant. Test sample reports are provided as a guide to clinicians to decide the significance of isolates when they are present in combination with other causative organisms.
- The right antibiotic treatment for the heavy growth of Staphylococcus aureus in a particular patient can be determined by sensitivity testing. This process can also help discover bacterial resistance to particular antibiotics.
- Labs are frequently unable to obtain accurate counts in samples with a heavy growth of Staphylococcus aureus, and the results are reported as “too numerous to count” (TNTC).
What Does Scanty Growth of Staphylococcus aureus Mean?
- In a bacteriology sample report, scanty growth of Staphylococcus aureus means that the bacterial colony found in the culture plate was that of the initial sample inoculum.
- A variety of factors can influence the amount of bacteria growth in a culture plate, including how well the swab was taken, prior antibiotic use, wound dressings, and so on. It does not always correspond to the patient’s level of infection.
- This invariably means that after incubating the culture plate for 24 or more hours, no growth was observed to establish evidence of infection, all other factors being accounted for.
- In a case such as this, another culture with a fresh sample has to be carried out in a non-fastidious medium to ensure the growth of other organisms that might be responsible for similar symptoms of infection.
- Treatment for scant growth of Staphylococcus aureus may not be needed, as there is no evidence of infection that could be established.
- To treat staph infections, doctors frequently administer cefazolin, nafcillin, oxacillin, vancomycin, daptomycin, and linezolid.
What Does moderate Growth of Staphylococcus aureus Mean?
- In a bacteriology sample report, moderate growth of Staphylococcus aureus means that the bacterial colony found in the culture plate was found occupying half of the plate.
- The amount of growth of the bacteria in a culture plate can be affected by a variety of factors such as how well the swab was taken, prior antibiotic use, wound dressings, and so on. It does not always correspond to the extent of infection in the patient.
- Treatment for moderate growth of Staphylococcus aureus: To treat staph infections, doctors frequently administer cefazolin, nafcillin, oxacillin, vancomycin, daptomycin, and linezolid.
Strains of Staphylococcus aureus
Methicillin-Susceptible Staphylococcus Aureus [MSSA]: These are rare antibiotic-resistant strains of
Staphylococcus aureus. They are resistant to a particular type of antibiotic (beta-lactam antibiotics).
This strain is usually associated with Staphylococcus aureus infections acquired in healthcare facilities.
Antibiotics that can treat the heavy growth of MRSA include Vancomycin and Daptomycin.
Vancomycin-resistant Staphylococcus aureus [VRSA]: it is possible for a patient to develop resistance
to the antibiotic Vancomycin. This is known as the VRSA strain.
Vancomycin resistance is rare, and mostly seen in patients undergoing long-term Vancomycin therapy. There are limited drugs available for the treatment of VRSA. Linezolid has proven to be effective in the treatment of VRSA.
Treatment of Heavy Growth of Staphylococcus aureus
Antibiotic Therapy
Antibiotics have been proven to be effective in the treatment of Staphylococcus aureus, however, there are different strains of Staphylococcus aureus and corresponding drugs effective in the treatment of these various strains.
Antibiotics available for the treatment of heavy growth of the various strains of Staphylococcus are:
- Quinupristin-Dalfopristin (Synercid): it is indicated for complicated skin and skin structure infection, intravascular catheter-associated bacteremia caused by Methicillin Susceptible Staphylococcus Aureus [MSSA].
- Dicloxacillin: Dicloxacillin is a penicillin antibiotic that treats MSSA and other Staphylococcal infections. It is effective for the treatment of pneumonia skin or soft tissue Staphylococcus infection.
- Nafcillin: Nafcillin is an antistaphylococcal drug. It is used to treat MSSA.
- Vancomycin: Vancomycin is an intravenous antibiotic. It has been shown to be effective in the treatment of Methicillin-resistant Staphylococcus aureus (MRSA). Vancomycin works by interrupting the cell wall synthesis in Staphylococcus Aureus.
- Daptomycin: Daptomycin is indicated for the treatment of complicated skin infections associated with Staphylococcus aureus. It is also used to treat MRSA.
- Linezolid: for patients who fail to respond to Daptomycin, Linezolid is an effective option. Linezolid has been shown to be effective against complicated skin and soft tissue infections, bone infections, and pneumonia.
Combination Therapy
Combination therapy is sometimes helpful in cases where Staphylococcus Aureus bacteria do not respond to standard antibiotic therapy.
- Cefazolin + Ertapene: the combination of ertapenem and cefazolin has been used in the successful eradication of Methicillin susceptible staphylococcus aureus (MSSA) bacteremia.
- Vancomycin + Flucloxacillin: combining vancomycin with flucloxacillin is an alternative strategy employed to improve the outcomes of MRSA bacteremia. There has been demonstrated synergy between Vancomycin and Flucloxacillin.
- Daptomycin + beta-lactam: there has been proven synergy in vitro activity against MRSA bacteremia in the combination of Beta-lactam to Daptomycin. This combination produced better results compared to when treatment was carried out with Daptomycin alone.
- Ceftaroline + Vancomycin: This combination may be used for patients that have shown MRSA bacteremia persistence when initial Vancomycin therapy was administered.
- Daptomycin + Oxacillin: the combination of Daptomycin and oxacillin showed improvement in vitro bactericidal effects. It is useful for the treatment of MRSA bacteremia.
What Next?
Staphylococcus aureus bacteria as present in either ‘heavy’ growth, ‘moderate’ growth, or ‘scanty’ growth is determined by the reports of the laboratory experiment.
From whence the appropriate treatment must be carried out using sensitivity testing.
