With the increase in drug resistance, allergic reactions, and side effects of some prescription drugs, an increasing number of people are looking for alternatives.
A major cause for concern is a study by the Centers for Disease Control and Prevention (CDC), which stated that each year more than 2 million people become ill from drug-resistant bacteria, resulting in 23,000 annual deaths!
Shortly, we will look at some of the possible natural remedies for E. coli infections.
E. coli infection
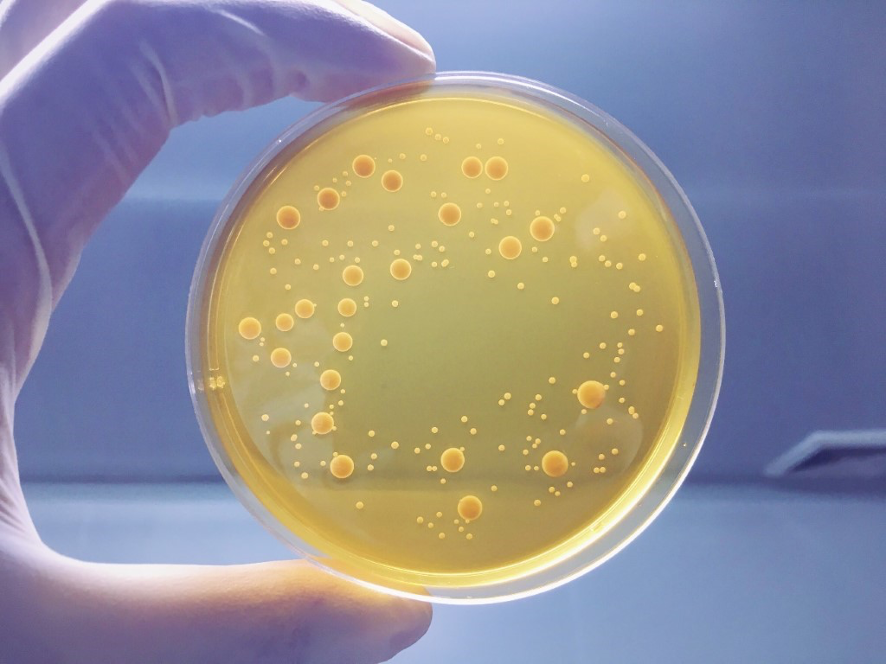
Escherichia coli (E. coli) is a gram-negative facultative anaerobic that lives normally in the gastrointestinal tract (GIT) of humans and animals. While most strains of E. coli are commensal, living harmlessly in the gut, some have virulence factors that make them pathogenic.
People are exposed to E. coli infection when they consume contaminated food (especially raw vegetables and undercooked meat); contaminated water; animals (especially people who work with animals like cows, sheep, and goats); and direct contact with a person that’s carrying the bacteria.
E. coli infections are often self-resolving, and many make full recoveries within days. However, it can get complicated for some vulnerable groups, like those with a weak immune system, young children, the elderly, and pregnant women.
If left untreated, an E. coli infection may progress to one of the following conditions:
- pneumonia
- urinary tract infection
- abdominal and pelvic infection
- a hemolytic uremic syndrome due to E. coli
- bacteremia, in which bacteria enter the bloodstream
- meningitis, in which bacteria cross the blood-brain barrier, or
According to the Centers for Disease Control and Prevention (CDC), about 5 to 10 percent of people with an E. coli infection develop hemolytic uremic syndrome (HUS), a condition that damages red blood cells.
This can lead to kidney failure, which may be life-threatening, especially for children and older adults. HUS generally begins about 5 to 10 days after the onset of diarrhea.
E. coli Treatment
In cases of E. coli-related diarrhea, it may be tempting to use an anti-diarrheal medication, but this is discouraged as diarrhea is one way the body rids itself of toxins. Preventing diarrhea, therefore, slows the process down.
Most doctors are hesitant to prescribe antibiotic medications to treat an E. coli infection. This is partly due to their risk of severe side effects and the buildup of antibiotic resistance, where antibiotics stop being effective against certain pathogens.
Also, taking antibiotics may increase the risk of hemolytic uremic syndrome (HUS). If a person develops HUS, hospitalization in an intensive care unit may be required. In such cases, treatment may include blood transfusions and kidney dialysis. According to the CDC, three to five percent of persons who develop HUS may die from this complication.
Lifestyle moderations like adequate bed rest and sipping fluids are often recommended to prevent dehydration and reduce symptoms while one recovers, especially for persons suffering from E. coli-induced diarrhea, since the illness is often self-limiting.
These recommendations include:
- Drinking clear liquids. Drink plenty of clear liquids, including water, clear sodas and broths, gelatin, and juices.
- Avoid apple and pear juices, caffeine, and alcohol. Whilst also
- Avoiding certain foods. Dairy products, fatty foods, high-fiber foods, or highly seasoned foods can worsen symptoms.
When one starts feeling better, one can return to a normal diet.
Alternative Natural Remedies for E. coli Infection.
A lot of research is going on as people seek alternatives to tackling illnesses and diseases and the growing incidence of drug resistance. Some of these efforts have been channeled into exploring some ancient natural remedies that have shown promise.
While some of these remedies have been used for hundreds of years, their efficacy has not yet been scientifically proven.
Some of the natural substances being explored that have shown antibacterial properties include:
- Garlic (Allium sativum L.)
Garlic has been used for centuries in various societies to combat infectious diseases. Historically, it is believed that Louis Pasteur described the antibacterial effect of garlic in 1858.
More recently, garlic has been proven to be effective against a plethora of gram-positive, gram-negative, and acid-fast bacteria including Salmonella and Escherichia coli.
One very good quality of ginger is its documented ability to exert differential inhibition between beneficial intestinal microflora and potentially harmful enterobacteria. The antibacterial activity of garlic is widely attributed to allicin, an organosulfur and defensive compound found in garlic with antioxidant and immunomodulatory effects.
- Ginger (Zingiber officinale)
Ginger belongs to the family of Zingiberaceae. It is widely used as an ingredient in food, pharmaceutical, cosmetic, and other industries. Ginger was proven to possess antimicrobial activities in several studies.
In their research, Indu et al. (2006) tested the antibacterial activities of 5 spice extracts against 20 serogroups of E. coli, 8 serotypes of Salmonella, L. monocytogenes, and A. hydrophila by the agar well method and filter paper method. The results indicated that ginger extract possessed inhibitory effects on two serogroups of E. coli.
- Honey
The medicinal importance of honey has been documented in the world’s oldest medical literature since ancient times. Honey has been known to possess antimicrobial properties as well as wound-healing abilities.
The first written reference to honey, a Sumerian tablet writing, dating back to 2100-2000 BC, mentions honey’s use as a drug and an ointment. Aristotle (384-322 BC), when discussing different jars of honey, referred to pale honey as being “good as a salve for sore eyes and wounds”.
The healing property of honey is due to the fact that it offers antibacterial activity, maintains a moist wound condition, and its high viscosity helps to provide a protective barrier to prevent infection.
The enzymatic production of hydrogen peroxide in most honey also confers them with antimicrobial abilities. However, another kind of honey, called non-peroxide honey (viz., manuka honey), displays significant antibacterial effects even when the hydrogen peroxide activity is blocked.
Its mechanism may be related to the low pH level of honey (honey is characteristically acidic, with a pH between 3.2 and 4.5, which is low enough to be inhibitory to several bacterial pathogens) and its high sugar content (high osmolarity) that is enough to hinder the growth of microbes.
Currently, many kinds of honey are sold with standardized levels of antibacterial activity, of which the best known are manuka (Leptospermum) honey and tualang (Koompassia excelsa) honey.
In research conducted on manuka (L. scoparium) honey, the honey was demonstrated to be effective against several human pathogens, including E. coli. Manuka honey has been widely researched and its antibacterial potential is renowned worldwide.
The potency of other kinds of honey, such as Tualang honey, against microorganisms, suggests their potential be used as an alternative therapeutic agent. The growth of bacterial species that cause gastric infections, such as S. typhi, S. flexneri and E. coli, have been shown to be inhibited by Tualang honey at low concentrations.
- Probiotics
Probiotic mechanisms are diverse, ranging from direct action against microbial pathogens through the antimicrobial action of bacteriocins and competitive exclusion of pathogens, to interactions with host cells by altering their responses to invading pathogens.
There are some studies that have shown promise in the use of probiotics to cure E. coli infections. Though the studies are in vitro, they have shown that probiotics may be useful in controlling infections caused by the SPEC variant, 0157:H7 in all three levels of microbial interaction, epithelium interaction, and immune system interaction.
Bifidobactecrial and Lactobacillus have shown the most potential in this regard. Though the results were not obtained from experiments on humans, with the positive signs shown, they could be extrapolated. This calls for more research in this area.
The probiotic bacterium, Lactobacillus, is a highly versatile genus of lactic acid bacteria comprising several strains with probiotic properties, used for a variety of ailments including gastrointestinal and urogenital diseases.
Lactobacillus rhamnosus GR-1 has been found to be helpful in maintaining urogenital health because of its efficacy in modulating the host immune system. This has proven to be effective in controlling UTIs and their primary causative agent, E. coli.
It is important to note that even with the opportunities they offer, these natural remedies also carry risks. The fact that a supposed remedy is labeled “natural” doesn’t necessarily mean that it is harmless. Knowledge of concentration and dosage should also be taken into consideration.
For example, while cooked garlic is usually safe to consume, research suggests that taking concentrated garlic may increase the risk of bleeding, which can be dangerous for people facing surgery or taking blood thinners.
Hence, it is pertinent that one consults with their healthcare provider before taking any such alternatives.
